Key points
- Anthrax can cause serious disease and death if not treated quickly after symptoms develop.
- Prophylactic antibiotics should be administered immediately to patients who might have been exposed to anthrax.
- Anthrax exposure is rare in the U.S., but some activities can put people at greater exposure risk.
- Anthrax is not contagious.
Overview
Anthrax is a serious infectious disease caused by Bacillus anthracis bacteria. It occurs naturally in soil and commonly affects domestic and wild animals around the world. People can also contract anthrax if they are exposed during a bioterrorism event.
Anthrax can cause severe illness in both people and animals. Anthrax is not contagious. It is very uncommon for people in the United States to be exposed to and become ill with anthrax.
How people contract anthrax
People can contract anthrax if they:
- Come in contact or work with infected animals or contaminated animal products (including hides)
- Consume food or water contaminated by B. anthracis
- Are exposed to anthrax in a laboratory that handles anthrax
- Are exposed during a bioterrorism attack
Certain activities can also increase a person's chances of exposure and infection to B. anthracis.
Types of anthrax
The type of illness a person develops when they have anthrax depends on how anthrax enters the body: through the skin, lungs, or the gastrointestinal tract. All types of anthrax can eventually cause systemic illness and death without antibiotic treatment.
Cutaneous anthrax
This most common form of anthrax infection occurs when anthrax spores get into the skin, usually through a cut or scrape. This form of anthrax is also considered to be the least dangerous. Infection usually develops from one to seven days after exposure. Exposure can happen when a person handles infected animals or contaminated animal products like wool, hides, or hair. Cutaneous anthrax is most common on the head, neck, forearms, and hands. It affects the skin and tissue around the site of infection.

Without treatment, up to 20 percent of people with cutaneous anthrax die. With appropriate antibiotic treatment, almost all patients with cutaneous anthrax survive.
Another type of anthrax exposure, called injection anthrax, has been found in other countries in people who inject drugs. This type of infection is similar to cutaneous anthrax but has areas of infection deep in the skin. Injection anthrax has never been reported in the United States.
Inhalation anthrax
This deadliest form of anthrax occurs when a person breathes in anthrax spores. Infection usually develops within a week after exposure, but it can take up to two months.

People who work in places such as wool mills, slaughterhouses, and tanneries may breathe in the spores when working with infected animals or contaminated animal products. Inhalation anthrax starts primarily in the lymph nodes in the chest before spreading throughout the rest of the body, ultimately causing severe respiratory distress and shock.
Without treatment, inhalation anthrax is almost always fatal. However, with aggressive treatment, about 55 percent of patients survive.
Gastrointestinal anthrax
This form has rarely been reported in the United States, but it occurs when a person eats raw or undercooked meat from an animal infected with anthrax. Once ingested, anthrax spores can affect the upper gastrointestinal tract (throat and esophagus), stomach, and intestines, causing a wide variety of symptoms. Infection usually develops from one to seven days after exposure.
Without treatment, more than half of patients with gastrointestinal anthrax die. However, with proper treatment, 60 percent of patients survive.
Symptoms
The symptoms of anthrax depend on the type of infection and can take anywhere from one day to more than two months to present. All types of anthrax have the potential, if untreated, to spread throughout the body and cause severe illness and death.
Cutaneous anthrax symptoms can include:
- A group of small blisters or bumps that may itch
- A large amount of swelling that can occur around the sore
- A painless skin sore (ulcer) with a black center that appears after the small blisters or bumps
- Most often the sore will be on the face, neck, arms, or hand
- Most often the sore will be on the face, neck, arms, or hand
Inhalation anthrax symptoms can include:
- Fever and chills
- Chest Discomfort
- Shortness of breath
- Confusion or dizziness
- Cough
- Nausea, vomiting, or stomach pains
- Headache
- Sweats (often drenching)
- Extreme tiredness
- Body aches
Gastrointestinal anthrax symptoms can include:
- Fever and chills
- Swelling of neck or lymph nodes
- Sore throat
- Painful swallowing
- Hoarseness
- Nausea and vomiting, especially bloody vomiting
- Diarrhea or bloody diarrhea
- Headache
- Flushing and red eyes
- Stomach pain
- Fainting
- Abdominal swelling
Diagnosing and treating anthrax
Healthcare providers in the United States rarely see a patient with anthrax. CDC guidance is available to help doctors diagnose anthrax, take patient histories to determine how exposure may have occurred, and order necessary diagnostic tests.
The only ways to confirm an anthrax diagnosis are to:
- Measure antibodies or toxin in blood
- Test for B. anthracis in blood, skin lesion swab, cerebrospinal fluid, or respiratory secretions
If inhalation anthrax is suspected, chest X-rays or CT scans can assist with diagnosis if the patient has commonly associated signs including mediastinal widening or pleural effusion.
Patient samples should be taken before the patient begins taking antibiotics if it does not delay the start of treatment.
Anthrax post-exposure prophylaxis and treatment
Patients with serious cases of anthrax require hospitalization. They may require aggressive treatment and supportive care, including continuous fluid drainage and mechanical ventilation.
Antibiotics
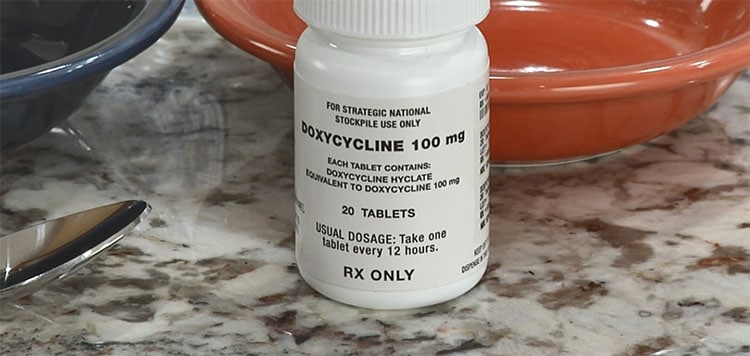
Antibiotics can be used for post-exposure prophylaxis (PEP) to prevent anthrax from developing in people who have been exposed but have not developed symptoms. All types of anthrax infection can be treated with antibiotics. Two of the most common antibiotics given to prevent and treat anthrax infection include:
- Ciprofloxacin
- Doxycycline
These antibiotics offer the same protection against anthrax. Anthrax spores typically take one to seven days to be activated, but some spores can remain dormant for up to 60 days or more before they are activated. Therefore, PEP for anthrax includes 60 days of antibiotics.

Antitoxin
Severe illness can occur if treatment is delayed because the patient didn't know they were exposed to anthrax. After anthrax toxins, which are released when anthrax spores are activated, have been released in the body, one possible treatment is anthrax antitoxin. Doctors must use antitoxin together with other treatment options, including antibiotics. Currently, there are a few types of antitoxins that can be used for treating anthrax.
Anthrax Reporting
Anthrax is a reportable disease in all U.S. states and territories. Anthrax cases must be reported to state and territorial jurisdictions when identified by a healthcare provider, hospital, or laboratory. Specific requirements for who must report cases and when to report vary by jurisdiction.
When immediate care is needed
Resources
Surveillance
- Anthrax Case Surveillance
- National Notifiable Diseases Surveillance System: Anthrax Case Definitions (2018)
- Medical Examiners, Coroners, and Biologic Terrorism (2004): A Guidebook for Surveillance and Case Management
Testing and diagnosis
- Recommended Specimens for Microbiology and Pathology for Diagnosis of Anthrax
- National Institute for Occupational Safety and Health: Worker Safety
Medical countermeasures, treatment, and PEP
- Clinical Framework and Medical Countermeasure Use During an Anthrax Mass-Casualty Incident: CDC Recommendations (2015) [PDF – 28 pages]
- Anthrax Vaccination: Information for Healthcare Professionals
- Vaccine recommendations for travel and some specific groups
- Antimicrobial Treatment for Systemic Anthrax: Analysis of Cases from 1945 to 2014 Identified Through a Systematic Literature Review (2015) [PDF – 10 pages]
- Antitoxin Treatment of Inhalation Anthrax: A Systematic Review (2015) [PDF – 13 pages]
- Prevention and Treatment of Anthrax in Adults (2023): Results of CDC Expert Panels
- Emergency Use Instructions (EUIs) for Antibiotic Post-Exposure Prophylaxis (PEP) of Anthrax
- CDC Guidance (2013): Anthrax Vaccine Adsorbed (AVA) Post-Exposure Prioritization [PDF – 19 pages]
- Guideline for Isolation Precautions (2007): Preventing Transmission of Infectious Agents in Healthcare Settings [PDF – 219 pages]
Other
