Protect Your Family: Reduce Contamination at Home
1997
DHHS (NIOSH) Publication Number 97-125
The National Institute for Occupational Safety and Health (NIOSH) is part of the Centers for Disease Control and Prevention (CDC) within the Department of Health and Human Services. NIOSH is the federal Institute responsible for conducting research and making recommendations for the prevention of work-related injuries and illnesses.
Disclaimer: Mention or implication of any company name or product does not constitute endorsement by the National Institute for Occupational Safety and Health.
NIOSH encourages the photocopying and distribution of all or part of this booklet to all those involved with hazardous substances.
The PDF version is also available. (16 pages, 202K).
Introduction
Workers can carry hazardous substances home from work on their clothes, bodies, tools, and other items. Workers can unknowingly expose their families to these substances, causing various health effects. This can also occur when the home and workplace are not separated, such as on farms.
The National Institute for Occupational Safety and Health (NIOSH) conducted a study of contamination of workers’ homes by hazardous substances transported from the workplace. The study documented cases of home contamination from 28 countries and 36 states in the United States. Reported cases cover a wide variety of materials, industries, and occupations.
About the Study
Why was the study done?
The Workers’ Family Protection Act of 1992 (Public Law 102-522, 29 U.S.C. 671a), directed the National Institute for Occupational Safety and Health (NIOSH) to study contamination of workers’ homes by hazardous substances transported from the workplace.
Other federal agencies that assisted NIOSH in conducting the study, include the:
- Agency for Toxic Substances and Disease Registry;
- Environmental Protection Agency;
- Occupational Safety and Health Administration;
- Department of Energy;
- Mine Safety and Health Administration; and
- Centers for Disease Control and Prevention.
How was the study done?
NIOSH obtained information for the study:
- through requests for information published in the Federal Register and CDC’s
Morbidity and Mortality Weekly Report; - from federal and state agencies and programs;
- from county agricultural extension agents;
- from Poison Control Centers;
- through letters to professional associations; and
- from published reports.
NIOSH published the report of this study in September 1995. It includes:
- a summary of incidents of home contamination;
- a survey of reported health effects;
- information on sources and levels of contamination;
- information on prevention and decontamination;
- a summary of relevant federal and state laws; and
- a description of responses by federal and state agencies and industry to incidents of workers’ home contamination.
What are the study’s limits?
The available information does not provide a basis for estimating the magnitude of the problem.
Few studies document the frequency and distribution of health effects among the families of workers in different occupations.
No surveillance system exists to record or monitor such cases.
Some conditions caused by worker home contamination are common (such as rashes and asthma) and may not be recognized as coming from work.
For many conditions, a long time passes between exposure to the material and the beginning of the condition. This makes it difficult to know the cause of the condition.
Existing reports contain little information about the levels of contamination in workers’ homes.
Contaminants
NIOSH found reports of incidents in 28 countries and 36 states. Such incidents have resulted in a wide range of health effects among workers’ families, including respiratory problems, neurologic disorders, and fatal poisonings. About half of the reports have appeared in the last 10 years.
Contaminants that caused health effects have among workers’ families include:
- beryllium
Nearly 40 reported cases of chronic beryllium disease were identified among workers’ families. - asbestos
Asbestos reaching workers’ homes has occurred worldwide, resulting in all forms of asbestos disease among workers’ family members, including over 100 identified deaths from mesothelioma in the United States. Although asbestos is now used less and regulated more, there is still the chance for exposure among workers’ families, especially among construction workers. - lead
Nearly 80 reported cases of workers’ family exposure to lead contamination were identified. More than half of the reports on workers’ children have occurred since 1990. - mercury
In six reported cases, workers’ homes were contaminated with mercury. The occupations of the workers involved included working at a chlor-alkali plant, the manufacturing of thermometers, and extracting gold at home. - arsenic
Arsenic in mine and smelter dust brought home on a worker’s clothing was considered a source of a child’s poisoning. - cadmium
Cadmium in the homes of lead-smelter workers resulted in increased levels in the workers’ children. - pesticides
Pesticide poisoning resulted in fatal and nonfatal cases in workers’ household members. Most reports occurred before 1980, but three more recent cases exist. - caustic farm products
More than 40 farm children have been poisoned by caustic farm products. - chlorinated hydrocarbons
Family members have been exposed when workers brought these substances home on their clothing. - estrogenic substances
Boys and girls have been affected by hormone-like chemicals brought home on the clothing of farmers and drug-company workers. - asthmagens and allergens
Family members have had allergic reactions to allergens from animals, mushroom farming, grain dust, and other materials. - fibrous glass
Family members have developed irritated skin after their clothing was washed with an insulation worker’s work clothes. - cyclothriethylenetriamine (RDX)
One child had epileptic seizures from this chemical brought home on a parent’s work clothes. - infectious agents
Family members have caught diseases such as scabies and Q fever from the clothing and skin of workers from hospitals, laboratories, and agricultural facilities.
Routes of Exposure
The means by which hazardous substances have reached workers’ homes and families include:
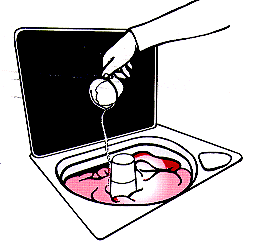
- work clothing
Cases involve beryllium, lead, pesticides, and other chemicals. In some cases washing machines and dryers contained dangerous levels of the materials, poisoning those laundering work clothes and contaminating other laundry. - tools and equipment
Substances brought home on hand tools and other equipment have contaminated homes and vehicles. Cases involved mercury, pesticides, PCBs, and radioactive material.
- taking items home from work
Items such as bags, rags, metal drums, and scrap lumber have caused serious and fatal poisonings of family members.
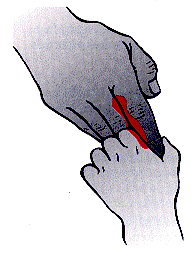
- the worker’s body
Reports document cases where workers passed dangerous materials to their family members by their hands.
- cottage industries
Twenty-two cases of contamination were found where work was done on home property. Contaminants included asbestos, lead, parathion, and mercury.
- farming
Several cases were found where families lived on the property where the farming was done. These involved pesticides, caustic substances, and a hormone-like chemical. - family visits to the workplace
Family members can be exposed to dangerous materials in dust or air through visits to work areas.
Prevention
For people who work away from their home:
- use good safety practices to reduce exposure;
- leave soiled clothes at work;
- change clothes before leaving work;
- store nonwork clothes away from work clothes;
- shower before leaving work;
- do not take tools, scrap, packaging, and similar items home;
- inform workers;
- launder work clothes separately; and
- prevent family members from visiting the work area.
For people who work in their home:
- keep work areas and living areas separate;
- keep family members out of the work area;
- store hazardous substances properly;
- dispose of dangerous materials properly;
- wash work clothes separately; and
- inform workers and household members.
Decontamination
Prevention is best. Decontamination is difficult and may not be effective.
Results depend on the cleaning methods used, the material to be removed, and the surface to be cleaned. Soft materials such as carpet and clothing are the hardest to clean. Lead, asbestos, pesticides, and beryllium are especially difficult to remove.
Normal house cleaning and laundry usually do not succeed. Sometimes, even the strongest decontamination methods fail. Decontamination may even increase the hazard to people in the home by stirring materials into the air.
Decontamination procedures include:
- air showers;
- laundering;
- dry cleaning;
- shampooing;
- airing;
- vacuuming; and
- other methods for cleaning surfaces.
Existing Federal Laws
Occupational Safety and Health Act
The Occupational Safety and Health Administration (OSHA) can
- require workers to wear protective clothing and remove contaminants;
- provide technical assistance that may help prevent home contamination; and
- directly set standards for workers’ homes if the workers are required to live in employer-provided housing.
The Federal Mine Safety and Health Act
The Mine Safety and Health Administration can
- make rules about protective equipment for miners (this can protect both miners and their families);
- require that employers provide facilities for employees to wash themselves and to change and store their clothes; and
- regulate home contamination if the mine is owned and operated by the miner.
Toxic Substances Control Act
The Environmental Protection Agency (EPA) can indirectly prevent home contamination through its authority to regulate chemicals and obtain information on their effects.
Asbestos Hazard Emergency Response Act
This act directly requires housekeeping, showers, and other practices to prevent exposure to employees’ families.
Residential Lead-Based Paint Hazard Reduction Act
This law has several parts that can help protect workers’ families, including:
- development of a standard for lead-contaminated house dust;
- development of a program to reduce exposure to lead;
- studies of lead exposure among children, including the potential for contamination from adults’ workplaces.
Comprehensive Environmental Response, Compensation, and Liability Act–Superfund Amendments and Reauthorization Act
This act regulates the release of hazardous substances to the environment from active and abandoned sites. Under it, the Environmental Protection Agency and the Agency for Toxic Substances and Disease Registry can consider workers’ contaminated homes as sites where hazardous wastes have been released, and limit and control contamination there.
Federal Insecticide, Fungicide, and Rodenticide Act
This act grants the Environmental Protection Agency authority to regulate the use of pesticides. The EPA has limited authority to prevent workers and farm owners from contaminating their homes.
Existing State Laws
Puerto Rico and the 30 states which responded to NIOSH’s request for information reported that they had no state laws that directly addressed protection of workers’ families. Some states do require reporting of cases of poisoning by lead and pesticides.
Employees can seek additional information from their employers. Employees and employers can both seek additional information from a health care provider skilled in occupational medicine, industrial hygiene, or a similar field.


